I worry about giving 30 million people a card and a false promise.[1]
—Dr. Atul Grover, Chief Public Policy Officer American Association of Medical Colleges
The Affordable Care Act of 2010 (ACA) is projected to expand health insurance coverage to an estimated 30 million to 34 million people. However, expansion of coverage is not an expansion of actual care, and the distinction is becoming clear.[2] When Congress enacted the national health law, it unleashed a potential tsunami of newly insured patients, flooding a delivery system that was already strained and fragile. The American health care infrastructure has had workforce shortages for decades and is not prepared to meet such a vast influx of patients effectively or efficiently. Training new physicians, nurses, and other health professionals takes years, sometimes decades. Without more graduates from nursing and medical schools and increased innovation in shared roles and responsibilities among doctors, nurses, and other medical professionals, individuals and families will face longer wait times, greater difficulty accessing providers, shortened time with providers, increased costs, and new frustrations with care delivery.
A system overload is inevitable. Pent-up demand from those waiting for a plastic card and attracted by the promise of “free” or heavily subsidized services is expected. Of course, doctors, nurses, and other medical professionals want to help people in need, but the sheer logistics of expanded care delivery, the current and growing shortage of personnel, and limited resources will certainly undercut the good intentions of the policymakers who crafted the national health law. In fact, the “transformational” changes touted by the law’s champions will likely complicate and negatively affect health care workers and their ability to provide care. These changes will increase regulatory burdens, increase already heavy workloads, reduce payments, impose new penalties, and disregard personal preferences and values. The increased stress will further destabilize the health care industry. These factors combined will threaten access and quality of care for all Americans, thus breaking the President’s promises and the stated intentions of those in Congress who enacted the national health law.
Making a Bad Situation Worse
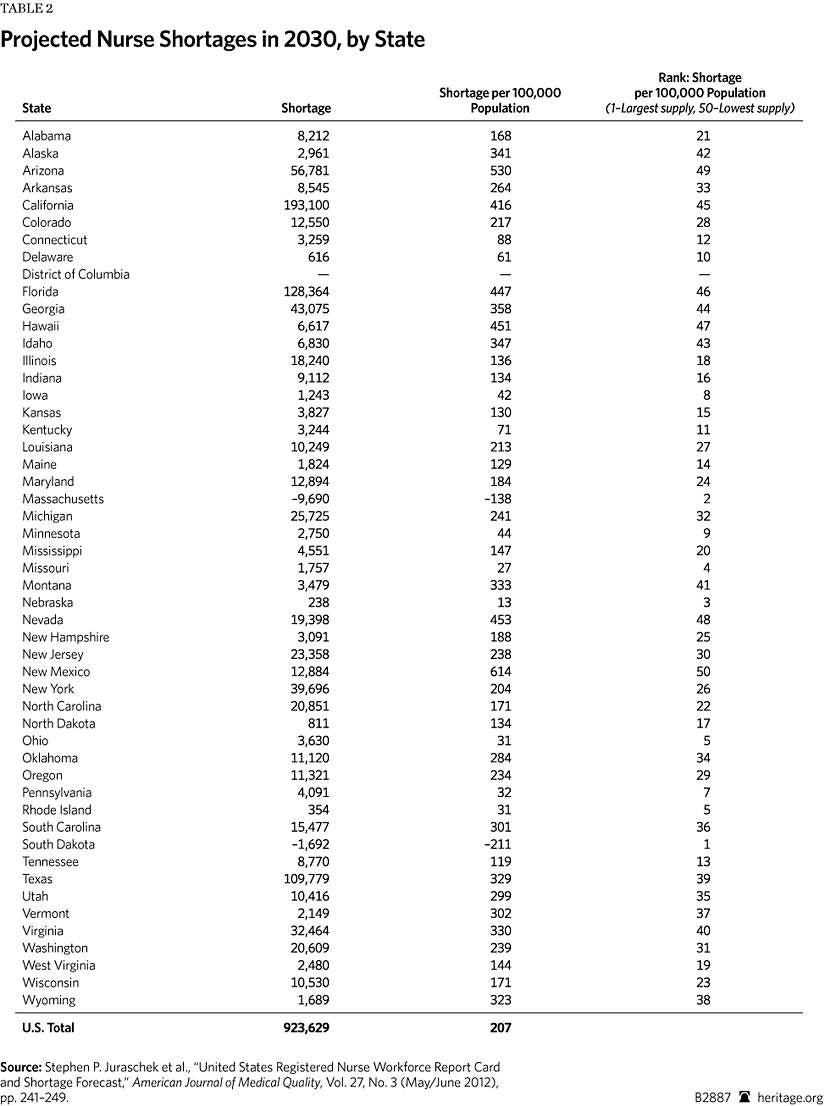
Despite the best efforts of medical professionals and educators to increase the workforce over the past few years, shortages are projected in every health care profession. The projected supply of workers fails to meet the demand associated with population growth and aging of the population. With the new demand for medical services for the millions who are expected to enroll in Medicaid and the federal and state insurance exchanges, the workforce shortages could become catastrophic.
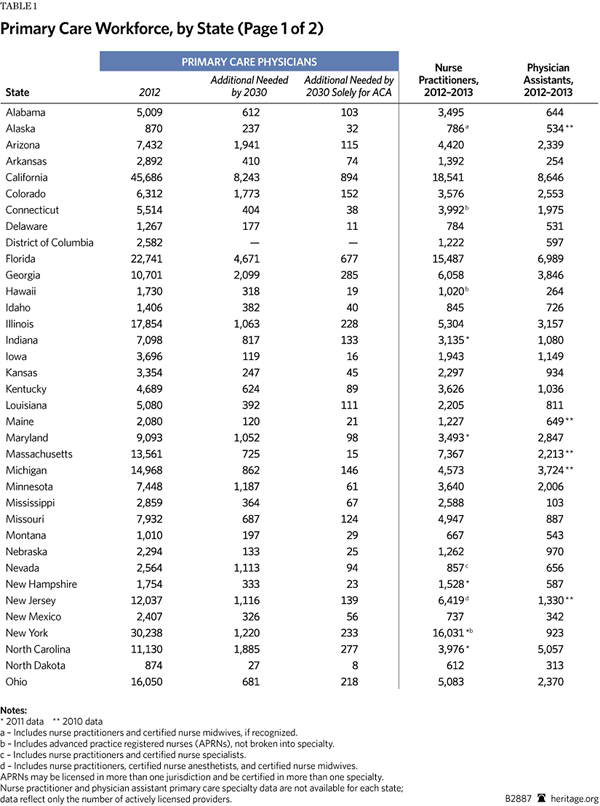
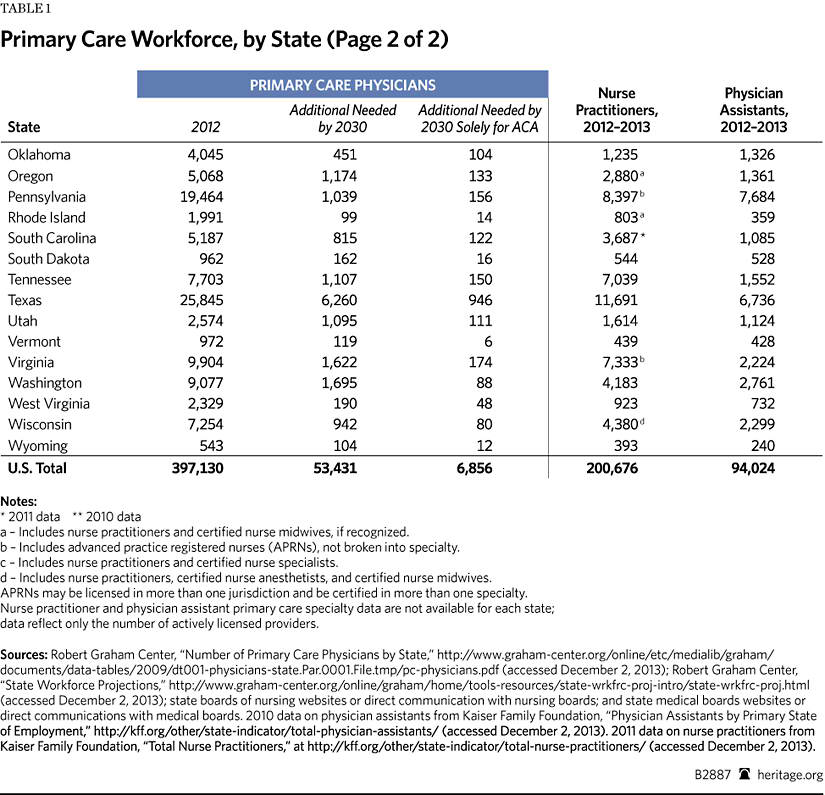
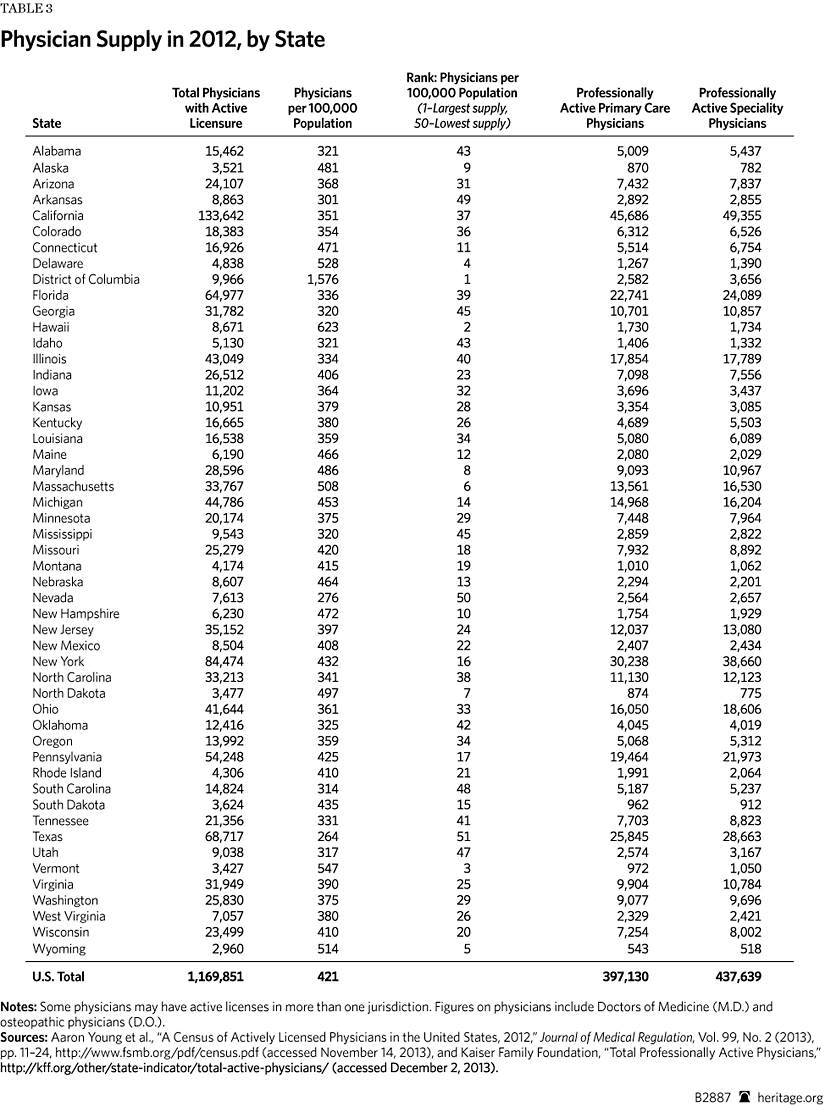
Based on a 2012 compilation of state workforce studies and reports, every state clearly needs more physicians. There are shortages of primary care physicians and specialists.[3] All health professions are facing personnel shortages: dental, mental health, pharmacy, and allied health—to name a few. Before the ACA’s enactment, a confluence of pressures had contributed to labor force problems. The ACA will impose additional strains on the health care workforce.
Population Demographics. The current U.S. population is more than 315 million and growing.[4] By 2030, 72 million Americans will be 65 or older, a 50 percent shift in age demographics since 2000.[5] The shift is mostly due to the aging baby boomers, who were born at the conclusion of World War II. Americans are living longer than ever before with the help of breakthroughs in medical technology and advanced care management. Seniors currently account for 12 percent of the population but will account for 21 percent by 2050. This growing, aging population will ensure more chronic disease and additional stress on the health care workforce.[6]
Distribution Shortfall. A maldistribution problem already exists. In much of the nation, health professionals are highly concentrated in urban locations.[7] The federal government established Health Professional Shortage Areas (HPSAs) in 1976, pursuant to congressional enactment of the Health Professions Educational Assistance Act, to increase the number of health care workers in rural and underserved areas. However, 37 years later, access to care is still unequal between urban and rural locations throughout the United States.[8]
The U.S. Department of Health and Human Services (HHS) projects the need for 7,987 primary care physicians in rural areas and shortages of dentists and psychiatrists as well.[9] Nationally, only 10 percent of physicians and 18 percent of nurse practitioners (NPs) practice in rural locations, yet one-fourth of America’s population resides in rural areas.[10] Rural populations are poorer and more likely to participate in government assistance, creating the potential for high demand due to the Medicaid expansion in 26 states.[11] Geographical challenges affect the health of rural Americans through longer wait times, difficulty accessing care, long-distance travel, and limited resources.
The ACA reauthorized loan repayment and forgiveness, scholarships, increases in Medicare-funded Graduate Medical Education (GME) residency slots, funding for workforce planning, and increased funding for the Public Health Service. These are intended to reduce the rural shortages, but these programs have historically achieved only limited success. Yet they have been the only initiatives to address maldistribution.
The danger is that these shortages will result in increased morbidity and mortality for rural Americans. Solving the problem will likely require a paradigm shift in educational admission practices, recruitment of more personnel with rural experiences, payment reform in the public and private sectors, and a much friendlier regulatory environment for medical practice, including tort reform.
Disproportionate Ratios. Another personnel supply problem is the disproportionate ratio of primary care physicians to specialists. Research suggests that the ideal ratio of specialists to primary care physicians is 40 percent to 50 percent in the healthiest nations.[12]A large gap in this ratio currently exists, with only one-third of physicians working in primary care. In states with higher ratios of specialists to primary care physicians, research indicates increased costs and decreased quality of care.[13]
The ACA relies heavily on the concept of the Patient Centered Medical Home (PCMH) model and free preventive care. However, both models require enough primary care providers to deliver services. This will be difficult given the projected personnel shortages.[14] The ACA’s newly insured population is expected to require at least 8,000 additional primary care physicians to meet their needs.[15] Even with the use of nurse practitioners (NPs) and physician assistants (PAs), projective shortages range from 20,400 to 45,000 primary care physicians over the next decade.[16]
Prospective medical students exhibit less interest in primary care in part because of a $3.5 million income gap over a lifetime of work and the increasing debt of student loans.[17] Primary care physician payments would need to increase by $100,000 annually to meet the income levels of specialists.[18] In both the public and the private sectors, medical professionals are taking advantage of payment reforms. Medical education should include new incentives for primary care. An emphasis on GME residency slots for primary care in the Medicare program might help to reverse the decline.[19]
Higher Intensity of Care. “Patient acuity” is a measurement of the intensity of care required to care for a patient. The higher the acuity, the more care a patient requires. In terms of work flow, this means the number of medical professionals needed to care for a patient depends on the gravity or nature of the patient’s medical condition. As the population ages, the number of patients suffering from chronic diseases will increase significantly, requiring additional labor hours to ensure quality of care. Furthermore, chronic disease is affecting more Americans, not just the elderly. By 2025, nearly half of all Americans will suffer from a chronic disease, resulting in a greater demand on the health care system.[20]
Looming Retirements. The aging population and aging workforce further complicate the ACA’s implementation. Of the estimated 2.8 million registered nurses (RNs) and the 985,375 physicians currently working, one-third will likely retire in the next decade.[21] Workforce projections anticipate a critical shortage of between 91,500 to 130,000 physicians and the need for an additional 300,000 to 1.2 million registered nurses by 2020.[22] The economic downturn of recent years has encouraged many professionals to stay in the workforce for financial reasons, but the additional stresses of the ACA will likely accelerate their exodus.
Younger physicians exhibit different attitudes toward their professional roles and responsibilities. A recent workforce survey described physicians over the age of 50 as more dedicated and hardworking and their younger counterparts as disillusioned, less dedicated, and not as hardworking.[23] If this survey accurately reflects the younger workforce, physician productivity will likely decrease with increased retirements. There is little hope of meeting expected demand if productivity and efficiency do not increase.[24]
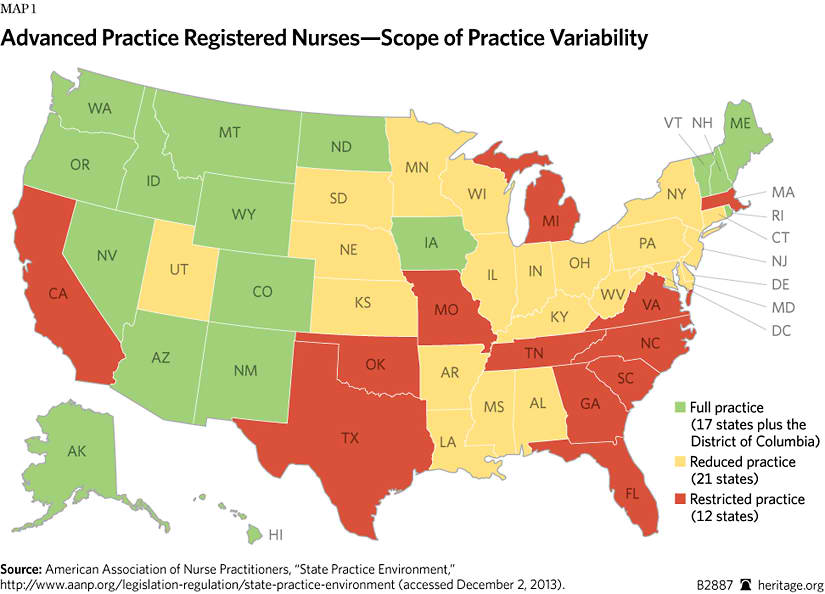
Scope-of-Practice Variability. In 2010, the Institute of Medicine (IOM) published a report recommending that all nurses practice to “the full extent of their education and training.”[25] Advanced practice registered nurses (APRNs) are not just NPs educated in primary care, but trained professionals who provide services in multiple specialties. Many are certified as nurse anesthetists, nurse midwives, and clinical nurse specialists. While PAs are defined as “part of a team” with supervising physicians, APRNS are trained to provide autonomous care for a focused population, such as primary care, pediatric, mental health, and critical care.[26]
Currently, scope-of-practice laws vary widely from state to state. Seventeen states and the District of Columbia allow full practice by APRNs without oversight by physicians. Another 21 states authorize reduced practice by allowing APRNs to practice in collaboration with a physician, and 12 states restrict practice requiring collaboration, oversight, and supervision by a physician.[27] The workforce shortage issue will require states to reexamine their scope-of-practice laws.
Educational Pipeline. Currently, medical education institutions are unable to graduate the number of workers needed to guarantee broad access to medical care. Even with recent enrollment increases, demand will still outweigh the supply by 2025.[28] The training pipeline is backlogged, and qualified applicants are not gaining entrance to professional schools. Insufficient numbers of instructors, limited clinical sites, and budgetary constraints contribute to the rejection of qualified applicants.[29]
Medical schools reportedly accepted 25,321 of 45,266 applicants in 2012 and are attempting to increase enrollment 30 percent by 2017.[30] While medical schools are increasing enrollment, the number of Medicare-funded GME slots is insufficient to complete the training process.[31] In 2012, the number of graduates exceeded residency slots for the first time. This shortfall will produce a snowball effect moving forward, creating yet another barrier to output.[32]
The American Association of Medical Colleges is supporting legislation to increase the number of Medicare-funded residency slots, but even if the President signs the legislation, the shortfall of residency slots will persist at least through 2017.[33] Even if medical schools can graduate more students, the lack of residency slots prevents graduates from practicing medicine.
Nursing is experiencing similar dynamics. More than 79,000 qualified applicants were turned away from nursing programs in 2012.[34] Complicating matters, the average salary for positions in nursing education is significantly lower than what these experts can earn outside academia, making it difficult to recruit and retain key academic personnel. A survey by the American Association of Colleges of Nursing identified 1,358 unfilled full-time faculty positions for the 2013–2014 academic year, and 414 schools reported full-time vacancies.[35]
Aging faculty also poses a threat to medical education. The average age of associate nursing professors is 52, and the average assistant professor is 49, while the average age of medical school faculty is between 50 and 59.[36] Retirements are on the horizon, and any additional losses of faculty will increase the backlog in the educational pipeline.
ACA Aggravating Workforce Stress
Without a strong and growing workforce operating under better working conditions, the quality of patient care will not improve. Health professionals worry about the ACA’s impact on their workforces, and many are considering alternative careers and opportunities. The ACA increases stress on individual workers, organizations, and systems. Part of the problem is the overwhelming complexity of implementing the massive law, requiring them to meet new legal requirements while fulfilling professional obligations and meeting professional expectations for high performance in delivering patient care. Rather than ease these problems, the ACA aggravates them.
Heavier Workloads. With millions of people entering the ranks of the insured combined with the decline in the growth of the health care workforce, doctors, nurses, and other medical professionals should expect their workload to increase dramatically. Increased safety issues and greater stress on workers will inevitably increase work demands.[37] The ACA’s financial incentives for and penalties against doctors and other medical professionals are to be tied to quality and performance metrics, but with the diminished workforce, maintaining the sufficient ratios to ensure quality care will be difficult.
Increased medical errors from fatigue, poorer outcomes, and even patient death are a direct result of workforce stress and heavy workloads.[38] Historically, vulnerable populations with complex medical conditions, such as the elderly and African Americans, are affected more. Heavy workloads can even increase health care disparities.[39] With the newly insured under the ACA anticipated to increase the number of patients in the system with complex medical issues, meeting their needs will require a significant investment of human capital. Otherwise, the additional strain will overwhelm already overstressed medical professionals.[40]
More Paperwork. In addition to the sheer number of new patients in the system, the ACA intensifies the regulation of an already overregulated system. The enormous paperwork requirements will reduce time spent with patients and significantly increase the costs of providing care. Complying with requirements to report quality measures and patient outcome data will require hiring additional staff and investing in infrastructure to complete the necessary tasks to ensure the highest level of payments.[41] After the 2006 Massachusetts health reform, the employment of administrative personnel in health care grew by more than 18 percent—a rate six times higher than the growth in employment of physicians and nurses.[42]
Since 1997, the federal government has issued 100 new or revised federal health care regulations, and this does not include countless state and local regulations. Medical professionals were already drowning in an ocean of paperwork. A 2001 study for the American Hospital Association found that hospital officials spent 30 minutes to one hour on paperwork for every hour spent on patient care in a Medicare-funded hospital.[43] For example, one hour of patient care in the emergency room required one hour of paperwork, and one hour of patient care in an acute care unit required 36 minutes of paperwork.[44]
The ACA has thus far added 109 distinct regulations. The time and effort to comply with these rules and regulations will equal an estimated 190 million hours of paperwork per year imposed on business and the health care industry.[45] Most of the estimated 13,000 pages of regulations are focused on health care institutions, and compliance with these rules will also reduce the time spent on direct patient care.[46] History suggests that this will cause a significant loss of direct patient care hours—a worrisome problem in light of the projected shortages and an unacceptable and unnecessary burden on the workforce.
Health care paperwork and government regulations are already out of control. Health care professionals went into medicine to help people, not to fill out government forms. Every minute and dollar spent on paperwork is a minute and dollar taken away from patient care. By adding 190 million hours of paperwork per year, the ACA will worsen practice conditions and exacerbate the health care workforce shortage, increasing costs and robbing health care professionals of the time needed to care safely for patients.[47]
The Penalty Problem. The ACA relies heavily on mandates, penalties, and bonus reimbursements for compliance with its regulatory standards. Even with attempts to improve performance over the past few years, 2,225 hospitals were penalized in 2013 under the Hospital Readmissions Reduction Program (HRRP), part of the ACA legislation. The penalties totaled more than $227 million, and facilities located in poor regions where a higher proportion of low-income patients are treated were hardest hit.[48] With the HRRP and the reduction of Medicaid Disproportionate Share Hospital (DSH) payments, providers are experiencing significant cuts in revenue while trying to increase quality of care to meet or maintain the ACA’s benchmarks. While physicians escaped a reduction in Medicare reimbursement rates in 2013, a 25 percent reduction is scheduled for 2014.[49] Under current law, physicians are unlikely to avoid the payment rate reductions, endangering their financial margins.
With the new regulations, lower reimbursement rates, and required investments in technology, health care institutions and medical professionals will have difficulty breaking even. In fact, hospitals laid off 6,000 workers in 2012, and more than 3,000 workers were affected by buyouts, attrition, or reductions in hours.[50]
The new pay-for-performance standards will significantly affect hiring and retention of labor. If facilities cannot improve their quality scores, the reduced reimbursements will mean budget cuts, shutting down units and even closing hospitals. A recent study indicated that hospitals were more likely to incur penalties when nurse staffing levels were lower, but the additional stress and strain combined with financial losses make reductions in workers likely.[51]
Increased Dissatisfaction and Burnout. Working in health care is difficult with adequate personnel, much less with the anticipated shortfall of workers. Increased work-related stress will affect the mental and emotional health of medical professionals.
In a recent survey, one-third of physicians would not choose medicine if given the choice to do it over again, and almost 60 percent would not recommend medicine as a career.[52] Physician well-being is directly correlated with the ability to provide quality of care to patients. With physician dissatisfaction increasing the likelihood of doctors leaving the profession by two to three times, Americans can expect additional labor losses.[53] The outlook is grim. A recent survey reported that 49 percent of physicians intend to stop practicing medicine as soon as possible or plan to reduce the years that they work in medicine.[54] Physician dissatisfaction, particularly burnout from overload and emotional stress, threatens reform efforts and patients’ access to care.[55]
Workplace stress is also responsible for depression and burnout among nurses. Nurses working in overcrowded and understaffed units are more likely to experience depression and absenteeism, thus increasing the burden on other nurses.[56] Nurses identify emotional distress from patient care, workload, fatigue, exhaustion, and an unfriendly workplace as reasons for leaving the profession.[57] The ACA does nothing to relieve this problem and may make it worse.
Medical Professionals’ Right of Conscience. Many health care professionals are concerned with profound moral and ethical issues that periodically arise in the health care field and worry about their traditional ability to exercise their rights of conscience under the ACA. This is not a new problem.
The Obama Administration all but rescinded the Bush Administration’s initiatives to protect health care workers. Thus, in many concrete circumstances, workers with religious or moral objections to certain medical treatments or procedures are left without specific, explicit protections, and the Obama Administration has thus far blocked legislation that attempts to correct the problem.
Current law contains no enforcement provisions. Meanwhile, HHS has blatantly disregarded right of conscience by mandating insurance funding of abortion-inducing drugs, contraception, and sterilization.[58] Right-of-conscience supporters have focused on reproductive rights and the rights of the unborn child, but the ethical concerns are broader. For example, these concerns can encompass anything that a medical professional or health worker finds to be a “major transgression” that is “well-defined” and “accepted by a cultural group.”[59]
Polling supports medical professionals’ ethical concerns. Right of conscience is supported by 63 percent of the American public, and 87 percent agree that health care workers should not be forced to participate in procedures that go against their moral conscience. In a survey of faith-based providers, 39 percent confirmed discrimination for using right of conscience and 95 percent indicated that they would leave the medical profession before they are forced to violate their conscience.[60]
ACA legislation creates a barrier to Medicare’s physician–patient relationship through the Independent Payment Advisory Board defining what treatments can or should be funded and insurance companies and government program officials determining what treatments are allowable. Health care workers are voicing growing concern over the implication of these barriers to ethical patient care. The marginalization of physicians and practitioners created by ACA legislation compromises safety and increasingly infringes on the ethical and moral obligations defined by the medical professions.
With the ACA-based contraceptive mandate and states considering measures to force health care workers to provide services regardless of moral objections, Americans have every reason to worry about efforts to violate the right to religious freedom and the right of conscience.[61] The health professions require workers to adhere to a code of ethics and to maintain the highest moral and ethical standards. Without explicit legal protections, health care workers will be forced to choose between violating their personal moral and ethical beliefs or losing their jobs. Without legislative guarantees and enforcement provisions, health care workers face discrimination.
The Effects on Health Care Delivery
In response to increased regulatory burdens, health care stakeholders are changing business practices. Ensuring viability in the new marketplace requires strategic planning and a vision of the future. A reevaluation of market standing, labor costs, and current infrastructure is essential to ensuring solvency as the ACA is implemented.
Mega Health Care. Hospitals, individual physicians, group practices, and other health care businesses are merging and consolidating to remain strong in the marketplace. Mergers and acquisitions reduce overhead costs for billing and claims while spreading out the financial risk and increasing market share. This gives them greater negotiating power with insurers, other hospitals, physicians, and government entities.[62] Horizontal and vertical consolidation in 2011 included 432 mergers involving 832 hospitals. At least 60 percent of hospitals are now in a system.[63] In Massachusetts, for example, conglomerates show lower costs of doing business but increased costs for consumers and insurers—a troubling trend if it holds nationwide.[64]
While alliances help to increase quality and efficiency through coordination of care, some argue that consolidation and mergers can also lead to monopolies in the marketplace. This raises anti-trust concerns. Consolidated systems may also lead to a reduction in quality as market consolidation eliminates the competitive incentives to improve care.[65]
Physicians are selling practices, moving into larger physician groups, and seeking employment at hospitals. Frustrated with increased regulation, the financial costs of practice, liability, continually increasing workloads, and the overall stress of the workplace, physicians are choosing to forgo independent practice. By 2011, 50 percent of physicians were working for hospitals, insurers, or corporations—a significant change in the landscape of care delivery of a magnitude not seen since the 1990s.[66] The shift of physicians to hospital payrolls increases operating costs while decreasing the bottom line and increasing prices for consumers and payers.[67]
Direct-Care Models. Legitimate concerns about the workforce shortage, burdensome regulations, reduced time with patients, and government involvement in the physician–patient relationship have prompted health care providers to begin changing independent practice models. Cash-only practices are popping up around the country with many posting price lists and requiring up-front payment for services. While the number of cash-only practices is small, practice conversions have been rising for the past few years. Physicians who follow this route significantly reduce overhead costs by eliminating patient billing and claims, freeing them to set their own prices and care for the patients in the manner that they see fit.[68] No insurance company or third party interferes with their decisions about treatments or care.
An estimated one-third of physicians were anticipated to move to such a subscription-based practice model by the end of 2013. Direct pay and “concierge care” are subscription-based models in which patients pay a monthly or annual fee. Fees vary widely depending on services provided. Concierge practices provide a higher level of service including care coordination and helping patients to negotiate the system while direct-pay practices provide more limited services, such as same-day appointments and additional access to doctors via phone or e-mail.[69] Patients pay a practice or membership fee with a contract between the physician and patient guaranteeing priority access and services added to basic care.
In most cases, patients are expected to retain insurance to cover fees for the physician’s basic services. Many of the practices accept private insurance, Medicare, and Medicaid. The HHS has warned about such practices in the past, and as the market for alternative access increases, there is concern that government will intervene to restrict or prohibit such practice models. Currently, as long as physicians can show that the services being paid for by the subscription fee are above and beyond the services that the physician is contracted to provide through the private insurance or government-run programs, they can avoid penalties for “double billing” or violations related to the insurance contracts.[70]
With subscription-based models, physicians can opt to limit or reduce the panel of patients allowing for individualized, unhurried care with a guaranteed baseline income. In fact, some insurance companies are building plans for employers that allow individuals to purchase the concierge option for increased access and payments.[71] While the cash-only, concierge care, and subscription-based models all attempt to safeguard the individual rights of the provider and patient while mitigating financial loss, the increasing number of these practices will affect affordability and accessibility for Americans. Innovative new practice models will guarantee access for those who can afford it.
Unintended Consequences. Adding up to 34 million patients to an insurance and delivery system that is already struggling with workforce shortages cannot avoid adversely affecting patient access and quality of care. The ACA cannot by itself guarantee access or increased quality of care through the mandated purchase of all-inclusive insurance policies. In fact, the unintended consequences of the ACA’s complexity will ripple throughout the health care sector.
Quality Health Care. Quality of care has been a major focus in health care in the U.S. for many years, and America’s medical professionals have continually tried to improve practice and provide the best care in the world. Nonetheless, the results have been uneven.
The ACA approach to guaranteeing quality is to move the medical workforce from the fee-for-service model of health care reimbursement to pay-for-performance. Pay-for-performance is an umbrella term for initiatives that give incentives or penalties measured by patient outcomes and readmission rates.[72] The research shows that the number of physicians in a state is associated with better quality and better outcomes.[73] As the workforce shortages worsen, the quality of care in states with fewer physicians overall will suffer. States with higher physician-to-resident ratios will fare better under the ACA’s pay-for-performance system, increasing inequality and disparity in the nation.[74]
While the concept of pay-for-performance shows some merit in reducing cost, transforming the system could prove difficult with the current penalties and reductions in reimbursement rates. Inadequate staffing levels significantly affect quality of care.[75] Low nurse staffing levels and higher nurse-to-patient ratios have been shown to increase morbidity and mortality.[76] Working conditions—such as increased pressure to perform, workforce shortages, and increased demand for services—will negatively affect health care institutions in the pay-for-performance system.
A recent survey reported that “40 percent of hospitalists are already seeing heavy workloads that result in unsafe conditions, delays in patient admissions and discharge, and failure to discuss treatment options.”[77] Hospitals and providers with more limited resources and medical professionals working in economically depressed areas may have difficulty meeting benchmarks of progress if their payments are further reduced under the ACA.[78] Strained finances, limited operating budgets, and staff layoffs—aggravated by ACA financial penalties and payment reductions—will cause a downward spiral of low performance. The Office of the Actuary in the Centers for Medicare and Medicaid Services, among others, has already projected that more hospitals will be operating in the red or hovering on the brink of insolvency.
Access to Health Care. Greater access to health care is a central ACA goal, but heavier demand for services will likely create a bottleneck in access. Individuals on the exchanges will likely experience a narrowing of networks and limited providers. In a survey by Jackson and Coker, 44 percent of physicians indicated that they will not participate in the exchanges.[79] A survey by the Medical Group Management Association found that 64 percent of practices are concerned with the regulatory burdens, and two out of three practices indicated that reimbursement rates were lower than commercial rates, heightening concern about participation. The negative impact on practice decisions and financial instability is motivating many physicians to avoid contracting with health plans in the exchanges.[80]
For example, a recent survey of 8,000 doctors in Massachusetts revealed a severe shortage that affected patient access to care.[81] Even though Massachusetts has one of the highest physician-per-resident ratios in the nation, the state needs an increase of 2.8 percent in the employment level of doctors and nurses to secure the requirements of the reform.[82] In a state that was better equipped to absorb the impact than most in the nation, worker shortages continue to inhibit access to care. States with a low physician-per-resident ratio (e.g., Nevada, Arkansas, Oklahoma, and Georgia) and states with more rural locations and limited access to the medical education pipeline will face critical shortfalls.[83]
Although many residents of urban areas may feel only a slight change, Americans living in more rural locations will bear the brunt of the shortage. Long waits will become common. In fact, wait times for new patients in some counties in Massachusetts have increased to 128 days for internists and 58 days for family practice physicians, leading to greater use of emergency rooms.[84] Half of primary care physicians are not accepting new patients, and the wait to see a gastroenterologist in Franklin County is 213 days.[85]
While many Americans will purchase insurance on heavily regulated exchanges, insurance itself does not guarantee access to or quality of care. Exchange plans with narrow networks invariably mean limited access to specialists and world-class treatment programs. Patients can lose choices in treatment and care.[86] Hospitals are closing, and rural hospitals and critical access facilities are increasingly at risk for closure. Many hospitals are requiring up-front payment of deductibles and co-pays for non-emergent services, further limiting access and delaying care.[87]
A New Health Care Agenda
The ACA requires millions of Americans to enroll in health insurance, but the care delivery system is unprepared to absorb the influx of Americans seeking care. The ACA’s new pressures will exacerbate attrition from burnout and dissatisfaction, worsening the existing shortage. Health care is a labor-intensive sector. The triple aim of increased quality and satisfaction, reduced costs, and increased health can be guaranteed only with an efficient workforce that is large enough to accommodate the needs of a growing and aging population.[88] Solutions to the existing problems will require innovation in medical education and training, improved delivery of care, and implementation of policies to retain the existing health care workforce.
Improve Education. Public policy is not the answer to all of the problems facing the medical professions. Many problems are endemic to professional training, and the terms and conditions of training and education should remain the responsibility of the professions.
Educational financing should reflect a better balance between primary care and specialty practices, increasing graduates of all health professions and providing financial incentives for faculty. If medical and other health care students seek relief to reduce the financial burdens of their professional education, they should expect to serve persons in areas with serious shortages of medical personnel. A 2013 medical school graduate accumulated an estimated $162,736 in debt by graduation. To make medical practice more attractive, policymakers need to address some pressing issues, such as limiting tort liability and other constraints created by the debt load.[89]
Medical and professional colleges should adopt admissions criteria that attract students from rural areas, and the curriculum should address the challenges of practice in a rural environment. Admissions officers should identify students from rural areas and those planning to practice in rural areas or primary care. Health professionals should incorporate interprofessional education to increase efficiency and productivity, promote coordination of care, and hold training exercises in teamwork. Increasing worker productivity will require strategic planning and partnerships to increase output of highly competent providers of care while addressing the maldistribution and disproportionate ratio of health care workers.
Congress should also reevaluate the current Graduate Medical Education program. It is imperative to ensure available residency slots for the projected medical student enrollment. GME strategic planning should focus on rural and underserved communities and create additional slots for specialties with the highest projected shortages, such as primary care.
Congress should also improve Title VIII Nursing Workforce Development. Programs funded through this initiative have contributed to an overall increase in the number of faculty and graduates of nursing schools.[90] Congress should evaluate the ACA’s Graduate Nurse Education (GNE) pilot program before providing additional funding. Future GNE programs should consider emphasizing rural education and primary care specialties to target specific distribution and shortage problems. Nursing educators need to streamline the curriculum to ensure that students are ready for work when they graduate.
As with many other areas of public policy, Congress should refrain from assuming responsibilities that are best left to state legislators, particularly where state nursing shortages are acute. In these cases, state legislators should set priorities and fund, as appropriate, nursing schools in their states based on their citizens’ needs.
Remove Barriers to Access. Scope-of-practice rules can contribute to the cost and inefficiency of the health care system, creating another barrier to patient access to care.
In a national survey of physicians and nurse practitioners, a majority of respondents indicated that having more nurse practitioners would improve timeliness of care and access.[91] A report commissioned by Massachusetts encouraged greater use of NPs and PAs, estimating that reducing restrictions would save the state $4.2 billion to $8.4 billion over 10 years.[92] While physicians are concerned with quality of care and, of course, a reduction in their market share, no evidence suggests that using APRNs negatively affects patients or physicians. Nursing, the largest segment of the health care workforce, should be “full partners” with other health professionals in the improvement of the health care system.[93]
Dr. Darrel E. Kirch, MD, chief executive officer of the American Association of Medical Colleges, recently stated that the medical community needs to train an additional 4,000 doctors per year “while also embracing the roles in which other professionals can serve.”[94] The impending shortage and the aging population demand a hard look at innovative models of care. The National Governors Association has come out in support of reexamining the scope-of-practice issues, and consumers are open to “a greater role for of physician assistants and nurse practitioners” in the health care system.[95]
Entrenchment of professional organizations has undercut reform in many states, even though the looming shortages will necessitate the full use of APRNs and other non-physician providers. Insurance companies and government agencies should remove obstacles to certification, eliminating payment issues. State legislators should examine the potential role of APRNs as a way to increase access and achieve additional savings. Given the current critical juncture of demand and supply of medical services, it is essential to ensure that all hands are on deck to care for the surge of patients.
Promote Efficient Care Delivery. Human capital is the backbone of the health care industry. Providing health care is labor intensive, and recruiting and retaining a sufficient workforce are essential. Strengthening the workforce supply should be coupled with innovation in role and task allocation.[96] Efficiency and productivity will expand the workers’ capacity to deliver high-quality patient care.
Achieving operational efficiencies among medical professionals will require systematic analysis.[97] To increase care coordination and improve work flow, professionals should pursue team-based collaboration.[98] This means health professionals should define the necessary tasks of their own professions and be ready and able to delegate tasks outside of their profession to other personnel. Workforce shortages compel health care leaders to invent new ways to use limited personnel efficiently to meet increased demands.
Improve the Practice Environment. Increasing retention will require greater incentives. Incentives should include a mix of public policies, such as reducing liability through tort reform, Medicare payment reform, and reduced federal tax rates. In the private sector, health care businesses will need to use the most effective methods of attracting, hiring, and retaining workers.[99] Retaining talent will require extensive human resource planning and incentivizing through benefits, education and career advancement, profit sharing, and workforce protections. Active interventions to prevent work overloads and strategies for stress management will reduce attrition and costly replacements and ensure adequate supply. Workers need to be protected physically, emotionally, and psychologically to ensure a healthy workforce.
Finally, health care workers should not be forced to choose between following their moral conscience and obeying potentially immoral orders of their superiors. Congress can contribute to workforce well-being by enacting legislation that explicitly guarantees the right of conscience and protects health care workers. Meanwhile, states should consider legislation that protects patients and workers from heavy workloads in state hospitals and other publicly funded institutions.
The Future of Health Care in the Balance
The viability of high-quality health care under the ACA is in doubt. The emerging health care workforce shortage, while rooted in trends that preceded the ACA, is not alleviated by the new health law. If these trends continue, they will become an insurmountable obstacle to the ACA’s success and damage the quality of care for millions of Americans. In short, Americans need more doctors, nurses, and other medical professionals.
Major provisions of the ACA were implemented in January 2014. With the rocky start to the exchange enrollment, the reduction in health plan competition in the exchanges, the emergence of narrow networks of doctors and other medical providers, and the rate shock of higher premiums and deductibles, more Americans oppose the new health law than support it. If these initial problems turn into cascading failures accompanied by massive disruptions of existing coverage and care, Congress will be forced to act.
Health care policy is no longer abstract when it directly affects the personal lives and health of millions of Americans. Under the ACA, Congress has prescribed a detailed federal role over health care financing, but financing directly and immediately affects the delivery of health care and how Americans access that care. Thus far, the ACA has delivered higher health insurance premiums, higher deductibles, and less competitive health insurance markets. This does not bode well for care delivery, particularly if it means increased waits, rationing of care, limited or no access, and poor quality of care. Americans’ private lives and their health decisions should be spared the consequences of such incompetent intrusions.
Sensible changes in health care policy could fix the problems of the few without harming the care of the many. Health care reform legislation should follow the principle primum non nocere (“first do no harm”) by carefully targeting the root of the problem, not by granting vast regulatory power to unaccountable government officials who issue arbitrary edicts.[100] Every day the ACA is the “law of the land” risks permanent damage to the health care sector of the economy and the lives of Americans.
There is no shortage of policy prescriptions for rational and profoundly consequential health care reform: portability of insurance, price transparency, tax reform, tort reform, deregulation, payment reform, and the elimination of artificial barriers to coverage and care. Meanwhile, the ACA’s unintended consequences cannot be ignored any longer. Americans should have the right of self-determination in health care. As the first step to secure that right, Congress must repeal this toxic law.
—Amy Anderson, DNP, RN, CNE, is a Graduate Health Policy Fellow in the Center for Health Policy Studies at The Heritage Foundation and an Assistant Professor of Nursing at the University of Arkansas at Little Rock.